Frequently Asked Questions
- What documentation is required for off-exchange Special Enrollment Period applications?
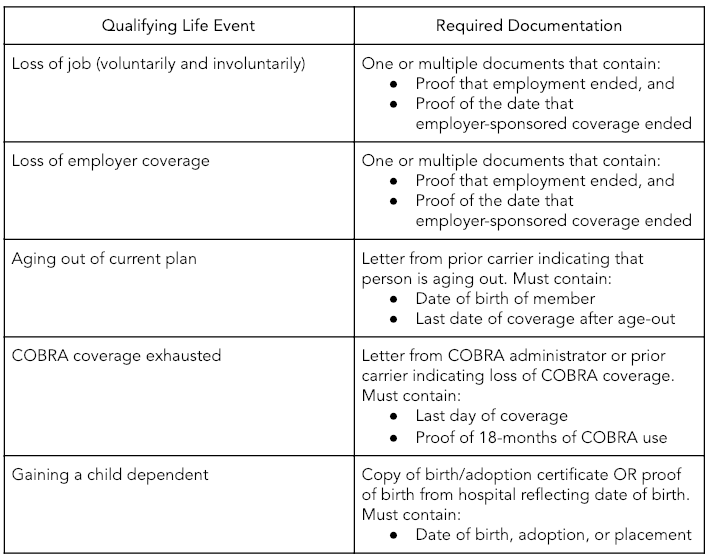
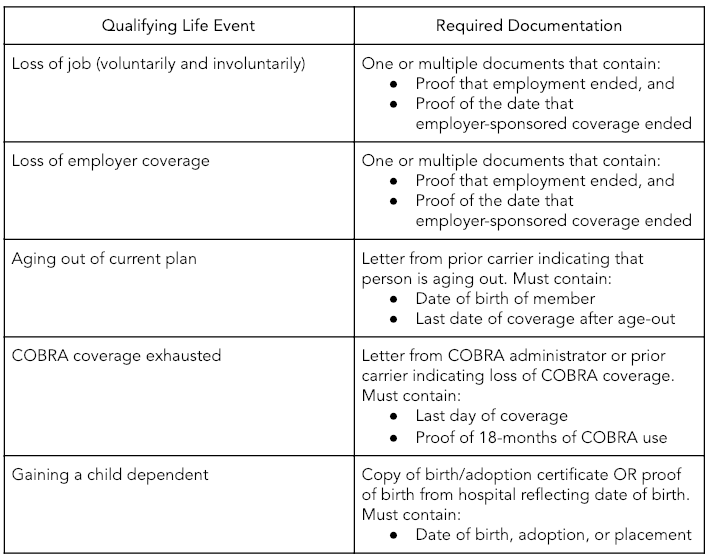
- When it comes to off-exchange Special Enrollment Period (SEP) applications, the required documentation will depend on the qualifying life event (QLE) that triggers the SEP. Here are the most common QLEs and the required documentation for each:
- Loss of coverage: Proof of loss and details of the member's previous coverage
- Change in household: Documentation for events like marriage, divorce, birth, adoption, or a death certificate
- Move to a new coverage area: A lease, mortgage, or USPS address change confirmation
- How long does a client have to enroll after a qualifying life event?
Your clients have 60 days from the date of their qualifying life event to complete enrollment. Be sure to submit all necessary documentation promptly to avoid any issues, such as application denials.
- If I’m enrolling an off-exchange client during the Special Enrollment Period, how long do I have to submit their qualifying documents?
You have 14 days from the effective date to submit your client's qualifying documents. Ensure these documents are dated within the last 60 days. For on-exchange policies, submit the documents directly to the exchange.
- If I do not submit the required SEP documentation during enrollment, how can I submit the required documentation?
- If you do not submit documentation during enrollment, you can email the qualifying documents to sepdocuments@hioscar.com within 14 days of the effective date.
- Do certain QLEs require more than one type of documentation?
No, each qualifying life event (QLE) requires only one type of documentation.
- When I upload my client’s QLE documentation via the upload function, will I receive any status updates?
You will only receive updates if the documentation doesn't meet requirements. Oscar will reach out via email within 5-7 business days providing information and requesting the proper documentation.
You can follow your client's enrollment progress via your Book of Business in your Broker portal.
- If I fail to upload my client’s QLE documentation during the time of enrollment and send via email, will I receive any status updates?
You will only receive updates if the documentation doesn't meet requirements. Oscar will reach out via email within 5-7 business days providing information and requesting the proper documentation.
You can follow your client's enrollment progress via your Book of Business in your Broker portal.
- What happens after my client or I submit an application for coverage during Special Enrollment Period?
You will only receive updates if the documentation is insufficient. Oscar will reach out to the broker via email within 5-7 business days detailing what's needed and requesting the proper documentation.
If the documentation is not accepted, you and your client will receive a cancellation notice via email with instructions on how to provide additional documentation and request reinstatement.
If no documentation is received following the enrollment, you and your client will receive several reminders to submit the appropriate documentation. If no documentation is received within 14 days, the enrollment will be canceled.
- Does ICHRA eligibility qualify as an SEP?
Yes, ICHRA eligibility qualifies as an SEP. This applies to individuals offered ICHRA coverage for the first time, as well as employees who previously had—or were offered—ICHRA coverage and chose to decline or end it.